Mupirocin, commonly referred to as pseudomonic acid A, is a topical antibiotic specifically designed to halt the growth of certain bacteria. It’s not a conventional first-line treatment for acne vulgaris, but it has a role in managing bacterial acne by blocking the proliferation of the bacteria responsible for the inflammation and skin lesions associated with this condition.
Navigating the landscape of acne treatments reveals various options, and while Mupirocin might not be the initial choice, understanding its appropriate use, the types available for acne management, and potential side effects is crucial. Moreover, recognizing alternative treatments can provide a broader spectrum of options for those seeking effective acne solutions without extensive risks.
Key Takeaways
- Mupirocin is a topical antibiotic that can intervene in bacterial acne but isn’t typically the first-choice treatment.
- Proper application methods and common types of Mupirocin for acne are important for effectiveness.
- Awareness of Mupirocin’s side effects and alternative acne treatments expands patient options.
Appropriate Usage
When managing acne with mupirocin, it’s pivotal that patients adhere strictly to the prescribed duration. Variances in treatment length can occur based on individual health assessments, hence the critical importance of following the guidance of a healthcare provider.
It’s vital to understand that mupirocin’s utility stretches only as far as the healthcare provider’s assessment deems necessary to combat bacterial influences on the skin. Given the interplay between ruptured pimples and the heightened risk for bacterial infections, mupirocin becomes instrumental in thwarting the propagation of these infections.
The use of Mupirocin in the context of acne treatment comes with various considerations regarding its effectiveness and potential concerns:
Bacterial Targeting
Mupirocin is effective against certain types of bacteria that may exacerbate acne conditions. It works by disrupting the replication process of these bacteria, thereby reducing their ability to cause infection and inflammation.
This targeted action makes it a useful option in cases where bacterial infection is a contributing factor to acne.
Variable Outcomes
The effectiveness of Mupirocin in controlling acne varies among individuals. While some may experience significant improvement, others may see less benefit.
This variability is a key consideration in its prescription, and it is often regarded favorably when other standard acne treatments have not yielded desired results.
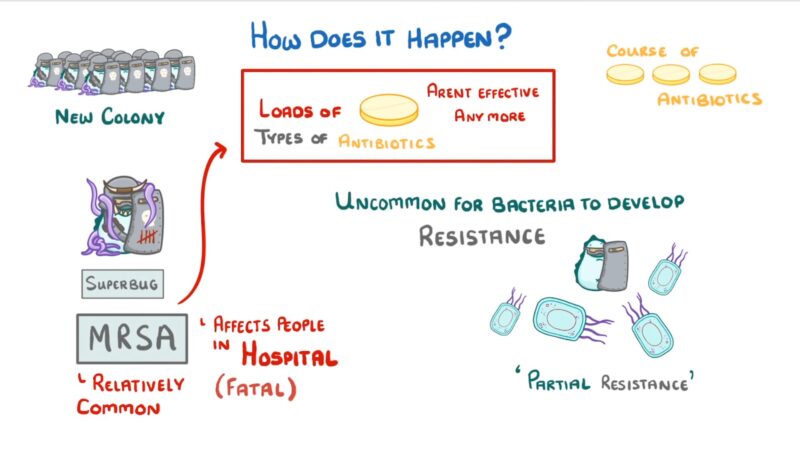
Risk of Resistance
Prolonged or inappropriate use can lead to the development of bacterial resistance. This is a significant concern as it can render the medication less effective against bacterial strains over time.
The emergence of resistant bacteria or opportunistic fungal infections is a risk associated with extended use, emphasizing the importance of following the prescribed duration and dosage.
Side Effects
Generally, Mupirocin is well-tolerated by most individuals. However, like any medication, it can have side effects.
Common side effects may include mild irritation at the application site, itching, or redness. More severe reactions, although rare, should be promptly addressed.
It’s crucial to consult with a healthcare professional before using this one. They can evaluate the potential benefits versus risks based on the individual’s specific skin condition and medical history.
Consideration for Combination Therapy
In some cases, it may be used as part of a combination therapy with other acne treatments. This approach can be beneficial in tackling various aspects of acne.
Healthcare providers may recommend combining Mupirocin with other topical or oral treatments to enhance overall effectiveness and address multiple factors contributing to acne.
Mupirocin Overuse
- Overuse of mupirocin may lead to fostering resistant bacteria, potentially inciting more severe forms of acne.
- Limiting usage to the prescribed duration is critical in preventing resistance and ensuring the maximum effectiveness of the treatment.
This approach offers a targeted approach to managing secondary bacterial infections associated with acne. However, effective use hinges on compliance with a healthcare provider’s recommended course of treatment, calibrated to individual needs and circumstances.
Prominent Mupirocin Variants for Acne Management
Mupirocin, commonly known for its pivotal role in addressing skin infections, is available predominantly in two formulations suitable for acne treatment: Bactroban and Centany. Both of these are topical treatments that leverage the efficacy of mupirocin to target the bacteria responsible for skin flare-ups.
- Bactroban: An ointment comprising 2% mupirocin as an uncombined acid, this variant is specifically crafted to tackle bacterial skin conditions. Its formula integrates oil and water to create a conducive base for the active ingredient, Mupirocin.
- Centany: This preparation is distinctively composed of 20 mg of mupirocin, combined with oleyl alcohol, castor oil, and other skin-compatible components. It is designed for external application and deemed safe for a broad age range, starting from as young as two months.
The nasal form of Bactroban, incorporating mupirocin calcium, serves a different purpose—targeting nasal bacteria—thus, is not typically prescribed for acne.
Mupirocin’s Additional Applications
Mupirocin, an antibacterial ointment, is effective against various bacterial infections.
This topical antibiotic is predominantly used for:
- Treating skin infections caused by specific bacteria
- Eradicating MRSA colonies from nasal passages
- Managing infections from antibiotic-resistant strains
Applying Mupirocin Effectively
- Preparation: Begin by cleansing hands with soap and water, ensuring they are completely clean before proceeding.
- Cleansing: Gently clean and pat dry the skin area where the ointment will be applied to remove any contaminants.
- Application: Utilize a sterile cotton swab to dab a modest quantity of the ointment onto the trouble spot.
- Dressing: If desired, one may lightly cover the ointment-treated area with sterile gauze to protect it, though this step is optional based on personal preference.
This topical remedy is generally recommended to be used three times daily, following storage guidelines to keep the ointment at room temperature. A noticeable improvement is typically expected around the fifth day of application.
In cases where no progress is observed, consulting a healthcare provider is advised.
Potential Adverse Effects of Mupirocin
We’ve mentioned the potential side effects, but now we want to discuss them in greater detail.
Medication Interactions with Mupirocin
Common Adverse Effects:
- Irritation: Patients may experience a mild sensation of burning or stinging.
- Skin Reactions: The appearance of blisters, rashes, or generalized itching is possible.
- Inflammation: Redness and swelling can occur at the site of application.
- Discomfort: There may be feelings of pain or tenderness.
- Skin Conditions: Symptoms can include cracked, dry, or peeling skin.
Patients should monitor these symptoms and consult a physician if they persist or worsen over time.
Less Common Adverse Effects:
- Oral Issues: Uncommon effects include sores, ulcers, or white spots in the mouth.
- Systemic Symptoms: These may include dizziness and symptoms resembling hives.
- Respiratory Problems: Difficulty breathing and general exhaustion may occur.
- Gastrointestinal Concerns: A serious condition involving C. difficile may cause blood or mucus in stool, persistent diarrhea, and stomach pain.
Allergic Reactions:
- Swelling in the mouth or throat, intense dizziness, rash, and respiratory issues can be indicative of an allergic reaction. Immediate medical attention is necessary if such symptoms occur.
Drug Interactions:
- It should not be used in combination with certain medications due to the risk of severe interactions. These medications include:
- Blood thinners such as Warfarin and Acenocoumarol.
- Other specific medications like Fluindione, Oxymetazoline, Estetrol, and Dicoumarol.
Patients must disclose their current medication list to their healthcare provider to prevent harmful drug interactions.
6 Alternatives to Mupirocin for Acne Management
Now, we want to explore some alternatives for this antibiotic you can use.
1. Triple Antibiotic Ointment
The triple antibiotic formulation, commonly found in over-the-counter solutions like Neosporin, guards against bacterial invasion in minor cuts and abrasions. Although it can alleviate redness and swelling related to acne, it does not address the underlying causes of acne itself.
2. Antimicrobial Peroxide Agent
Benzoyl peroxide is a go-to solution for controlling bacteria that cause pimples. It clears pores and minimizes oiliness, but its potent oxidizing effects can lead to skin dryness and irritation, suggesting its cautious use primarily as a targeted remedy.
3. Vitamin A Derivative
Topical retinoids, derived from Vitamin A, such as over-the-counter retinol or prescription-strength tretinoin, promote faster skin cell renewal. This process effectively diminishes most acne forms more efficiently than Mupirocin, which may only be preferred for bacterial-related acne conditions.
4. Combined Antibacterial Formula
Benzyamycin unites benzoyl peroxide with the antibiotic erythromycin to form a potent acne-fighting blend. This dual-action combats acne while mitigating antibiotic resistance, although it may induce sensitivity reactions and dryness.
5. Antibiotic Cream
The medicinal cream known as Cleocin, or by its generic name clindamycin, interrupts bacterial growth akin to Mupirocin. Despite its effectiveness against acne, users with sensitive skin might experience irritation.
6. Anti-infective Therapy
Vancocin tackles severe skin infections and certain resistant strains of bacteria. This makes it suitable for complex bacterial conditions beyond the typical scope of standard acne treatments.
Applications of Mupirocin Beyond Acne Treatment
Mupirocin, an antibiotic ointment, is utilized extensively for skin conditions other than acne. Recognized for its effectiveness against certain bacteria, it is often the medication of choice for:
- Treating Impetigo: This highly contagious infection predominantly affects young children, causing itchy sores and yellowish crusts primarily around the mouth.
- Controlling MRSA: In cases of methicillin-resistant Staphylococcus aureus, it’s applied inside the nose to reduce bacterial presence.
- Managing Minor Wounds: It’s beneficial for treating infected hair follicles, boils, and minor burns or scrapes to prevent secondary bacterial infections.
- Healing Traumatic Skin Lesions: With its ability to inhibit bacterial growth, it aids in the recovery of various skin ulcerations and lesions.
Use is typically restricted to ensuring that resistant strains of bacteria, such as certain Staphylococcus or Streptococcus species, do not develop.
Common Queries Regarding Mupirocin
Effectiveness of Mupirocin:
- Individuals generally observe improvement in their skin condition within a few days of initiating Mupirocin.
- By the tenth day, improvements should be substantial.
Mupirocin and Scarring:
- Mupirocin is effective in reducing inflammation, which can, in turn, decelerate the formation and visibility of scars.
Mupirocin vs. Neosporin:
- Mupirocin is a topically applied antibiotic often prescribed for bacterial skin infections like acne or Impetigo.
- Neosporin, conversely, is typically recommended for minor cuts and abrasions.
Diet and Acne Management:
- Beyond topical treatments, diet significantly influences skin health.
- A balanced diet can support efforts to achieve clearer skin.
- Notes for Specific Groups:
- Pregnancy: Seek medical advice before use.
- Breastfeeding: Consult a healthcare professional.
- Children: Check with a pediatric dermatologist for appropriate precautions.
- Further Precautions:
- Antibiotic Resistance: Use as directed by a healthcare professional to lower the risk of bacterial resistance.
- Missed Dose: If a dose is missed, apply as soon as remembered, but not close to the next scheduled time.
For personalized medical advice, always consult a dermatologist or other qualified healthcare professional.
FAQs
Efficacy of Mupirocin for Acne-Related Conditions
Mupirocin is typically prescribed as a bacterial infection treatment. It’s not the first-line treatment for standard acne but may be advised by a healthcare professional if a secondary bacterial infection is suspected within the skin. Which conditions warrant Mupirocin as an acne treatment?
Application of Mupirocin on Facial Skin
Direct application of Mupirocin to the face is generally considered safe if done so according to a doctor’s prescription. It should be applied in a thin layer to the affected area, ensuring the skin is clean before application. How should Mupirocin be applied to facial areas?
Mupirocin’s Interaction with Rosacea Symptoms
There’s limited data on the effects of Mupirocin on rosacea. Since rosacea is a chronic, inflammatory skin condition, and Mupirocin is an antibacterial ointment, it may not address the underlying causes of rosacea. Consult a dermatologist for tailored advice.
Timespan for Mupirocin to Exhibit Effects
The time Mupirocin takes to show improvement in skin conditions varies. Users often must continue treatment for a prescribed duration, even if symptoms seem to improve before completion. How long does it take for Mupirocin to work?
Mupirocin and Risk of Clogged Pores
Mupirocin itself is not implicated in pore blockage; however, any topical product has the potential to contribute to acne if it doesn’t suit an individual’s skin type. It’s best used under medical supervision.
Mupirocin’s Effectiveness on Fungally Induced Acne
Mupirocin is an antibacterial cream and therefore not intended for fungal infections. Acne-like fungal conditions require antifungal treatments, not antibiotics like Mupirocin. Can Mupirocin treat acne caused by fungi?
Closing Thoughts
While this antibiotic is not primarily designed for acne treatment, its role in skincare, particularly in addressing bacterial skin infections, cannot be overlooked. For those struggling with acne that is complicated by bacterial infections, it can offer a beneficial adjunct treatment under the guidance of a healthcare professional.
However, it’s important to understand that it should not be used as a first-line treatment for typical acne. Its usage should be reserved for specific cases where bacterial involvement is evident and diagnosed by a healthcare provider.